Virtual wards are a crucial part of NHS plans to increase capacity, as highlighted in the recent delivery plan for recovering Urgent and Emergency Care services (UEC). The “twindemic” (of Covid-19 and flu) has contributed to record levels of occupancy (as high as 95% across the country) which, combined with staff burnout, has made capacity in hospitals a critical bottleneck. To address this, one of the key interventions backed is the establishment of ‘virtual wards’ in the patient’s home, facilitated by remote monitoring, to avoid admission or allow earlier discharge. The benefits of such an approach are clear but they are complex to implement. There are multiple case examples of high impact implementation leading to reduced length of stay, reduced readmission rates and lower costs, whilst also improving patient satisfaction.
The scale of challenge in UEC and amount of investment make it vital that virtual wards are a success. It’s believed that, by Christmas 2022, 10,000 patients had used virtual wards and the government announced plans to increase this 500%. Anecdotally, however, existing capacity has not been fully utilised. £450m has been committed over 2 years to this programme, making it critical that virtual wards are effectively implemented and utilised.
We outline below the basis of what a virtual ward is and why we need them before turning to the questions of what is the track record and how we measure success? We also identify five drivers of a successful virtual ward programme: consultation, impact measurement, good use of technology, management of clinical change and the use of flexible workforce models.
What is a virtual ward?
Virtual wards are shorthand for additional remote care services in health and social care provided in a home setting which allow patients to get the care they need at home, safely and conveniently, rather than being in a hospital setting. Virtual wards became a crucial part of the 2022/23 NHS England operational plan, with a target of 40-50 beds per 100,000 population (equivalent to the delivery of up to 24,000 virtual ward beds in total) by December 2023[1]. To achieve this there is a recognition that the rollout of the virtual ward model will have to be innovative and make use of digital technology where possible.
Technology can provide the hardware and software to remotely monitor patients’ wellbeing. Clinicians can understand what is happening with their patients without needing to visit in person. Attention from multidisciplinary teams can then be focused on the patients with the greatest or most immediate need.
The Covid-19 pandemic necessitated a shift away from in-hospital care. Patients being cared for at home with additional services provided an example of how virtual wards can be used effectively. The success of these local services has led to national support for rolling out additional capacity in virtual wards; NHS England has committed £200 million through the Service Development Fund to develop virtual wards through 2022/23 and then a further £250m of matched funding for 2023/24.
Why do we need these services?
There is clear evidence that caring for people in their own homes supports their recovery. Patients prefer it because it enables more autonomy and choice whilst enabling them to stay in familiar surroundings, with their local support network (family, friends) often close by. In addition, studies have shown that virtual ward models significantly reduce attendance to Accident & Emergency departments and associated unplanned hospital admissions. This is because patient needs can be met earlier, before becoming a crisis, through the provision of multidisciplinary care[2].
Other studies have found that following the implementation of virtual wards, hospital re-admission rates reduced by 50%[3] and average length of a hospital stay was reduced by 40%[4]. Given physical capacity constraints in acute hospitals and ongoing constraints to capital availability in the NHS infrastructure and changing population demographics increasing demand, we must continue to find new and innovative ways to safely manage more patients within their own homes. This must include finding more effective ways to discharge into other settings of care.
What is required for implementation?
Central to implementing virtual ward programmes will be identifying and utilising effective digital solutions. Virtual wards require clinical oversight and, with the increasing workforce availability constraints, mean that remote monitoring and workforce optimisation solutions can help more people receive high quality care within an increasingly limited resource.
At present, there is a wide range of virtual ward services with variable use of technology. So far they are providing very effective personalised care, but the anticipated cost savings of providing a service at home versus hospital are still to be realised in full. Despite the comparatively high cost of acute hospital beds, home visits can be staff-intensive and the length of time people require care tends to be longer than in hospital, resulting in a smaller cost differential than anticipated. Incorporating digital solutions will help free up staff and increase the efficiency of the service, reducing costs.
Additionally, digital solutions can help support people’s overall health needs by improving the quality of care and patient experience. Research found that 99.5% of the patient cohort who received ‘virtual ward’ stays were likely or extremely likely to recommend virtual ward stays to family and friends. Studies also found that these service models also improve the experience of the workforce[5].
Implementing virtual wards effectively, with the right enabling digital services will help decrease the cost of care provision, whilst improving patient care, at home where they are comfortable. As such, it effectively responds to the Triple Aim of the NHS by improving: the health and well–being of the population; the quality of services provided; and the sustainability and efficiency of resource use. This should help focus minds on how best to advance the virtual wards agenda.
What are the complexities of delivery?
Ensuring that virtual wards are inclusive is a complex task. Virtual wards are designed to improve access to care for population groups which have traditionally been hard to reach, but there is a risk that they could reinforce existing inequalities in care provision by prioritising those who are more digitally literate. Therefore, it is important that technology is used and care is distributed equitably to ensure that these gaps are not widened[6]. This requirement will apply to the specific design of the monitoring technology, the approach to offering a wraparound service of support and communicating effectively with patients.
Community services will need to adapt to accommodate new ways of working as virtual wards and their workforce caseloads become a regular feature of health and social care. Whilst virtual wards will reduce pressure on in-hospital wards, they will also increase the caseload for the community workforce, so when implementing a virtual ward, it requires both implementing operational change and the digital tools to support them. This includes joint approaches across the care system on care model design and best use of scarce resources to create a service that can truly reduce pressures on the health and care system overall, rather than just transferring pressure from the acute to the community.
However, this can also be viewed as an opportunity. Virtual ward programmes offer clear opportunities to create innovative workforce models in the NHS and with social care. Many clinicians leaving the NHS cite a lack of flexibility in their work, but movements away from traditional expectations as virtual wards are implemented will allow for more flexible workforce programmes, potentially helping with retention. For example, virtual wards programmes might allow clinicians more opportunity to work from home.
Integrated Care Systems (ICSs) can help support different ways of working. Enabling staff, including community and hospital clinicians, to work across organisational boundaries within an ICS will be difficult but the rewards will be long lasting. These include improved patient and staff experience, as well as enhanced capacity within the NHS and social care. It is the responsibility of ICS leads to deliver against this ambitious transformation to improve care for patients and staff in the longer term.
What are the key drivers for success?
When setting up virtual ward programmes, several key drivers must be considered, to ensure that benefits are being realised. Virtual wards must be carefully tailored to the sector and area they serve.
Consultation – Local residents must be consulted with for consideration as to whether they will benefit from virtual ward care. Programme leads must engage clinicians with the requisite expertise on local populations and create patient groups that adequately represent the patient groups targeted by the new service.
Measuring impact – There is significant evidence that virtual wards have a positive impact, with an estimated £1,047 saving for each patient using a virtual ward[7] but this can be hard to assess given high occupancy in the acute sector at present. A patient using a virtual ward bed will free up a bed which will likely be occupied, rather than reducing occupancy in sum.
Technology – Given the benefits technology can bring to management of virtual wards, choosing the right technology partner is crucial, with different solutions appropriate for different ward types; for example, there is a balance between continuous monitoring and spot reporting. Engaging clinical teams to understand the needs of patients will ensure that the technology used is appropriate and effective for meeting patients’ needs. Consistent innovation will be needed to ensure that virtual ward delivery continually improves.
Managing clinical change – Those responsible for establishing virtual ward programmes must be cognisant that virtual wards increase patient acuity in the community and the associated risk must be proactively managed. For example, engagement with the local community combined with a tailored approach to the use of technology can minimise patient risk, whilst ensuring that patients who can safely remain out of hospital do so. Clear safety netting, consideration of the processes for out of hours care and well-defined routes of escalation will enable greater protection for these patients.
Flexible workforce models – Requires learning to adapt to new technologies, as well as novel ways of working making best use of multi-disciplinary teams. We must ensure that training is aligned to advances and changes in how care is delivered, so that all members of a multi-disciplinary team are equipped to deliver care in the best possible way.
Whilst technology is advancing to aid efficiency in care and providing patients with choice and flexibility in how they receive their care, we must be aware that human factors play a significant role in care delivery; a balance must be struck between technology and the human element of care.
However, creating capacity will not help resolve pressures in the NHS unless actually utilised. There must be an active effort to encourage utilisation of services and embed change, beyond the initial creation phase. Otherwise, additional virtual ward capacity risks underuse, a significant boost to capacity which is not taken advantage of.
How can CF support?
CF is an expert healthcare and analytics consultancy which is well-placed to help systems embrace and implement virtual wards. We bring a wealth of experience in the health and care space and can support virtual ward development. Our support includes:
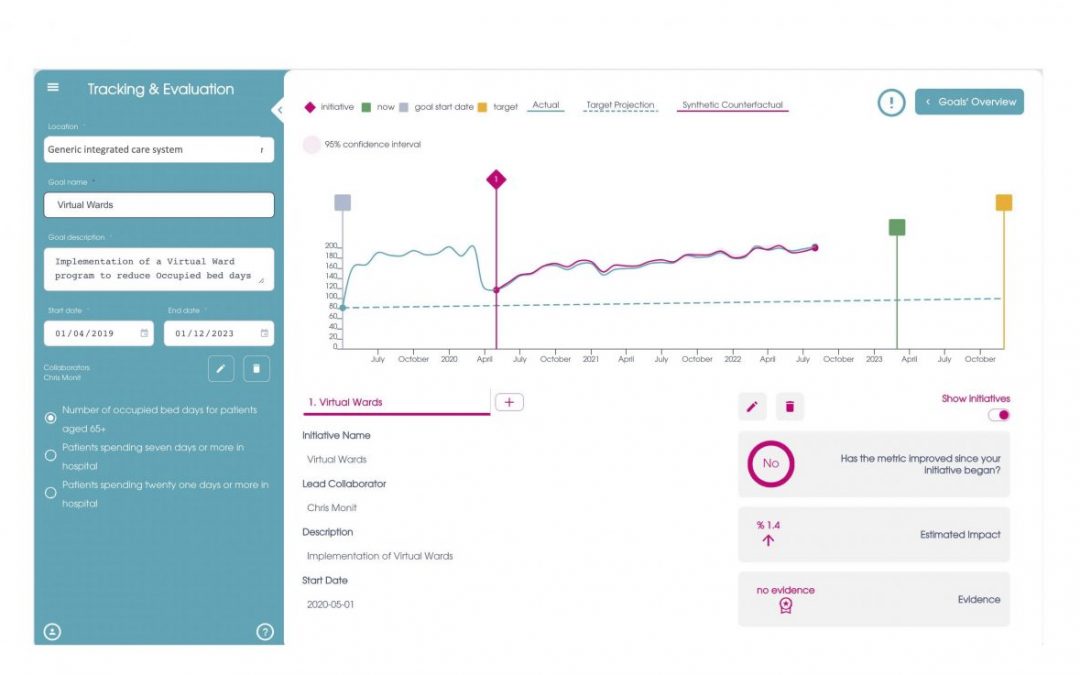
- On-course evaluation – CF can provide data innovation expertise, products, and solutions, including monitoring the benefits of virtual wards to patients. An example of the evaluation tool is provided below.
- Financial sustainability and planning – Use CF’s extensive financial expertise to understand the system impact of virtual wards and develop a sustainable funding model for the services.
- Digital adoption – CF can support the adoption of new technologies within NHS organisations and unlock the potential of digital solutions, understanding the remote monitoring requirements and needs for digital inclusion.
- Clinical engagement – We can link digital capabilities with deep clinical insight to provide a holistic approach and support clinicians to adopt virtual wards as part of new approaches to emergency care.
- Change management – We can provide expert input to support a change management programme into the new ways of working.
- Programme oversight – We can lead virtual ward change and support programmes to delivery against ICS planning.
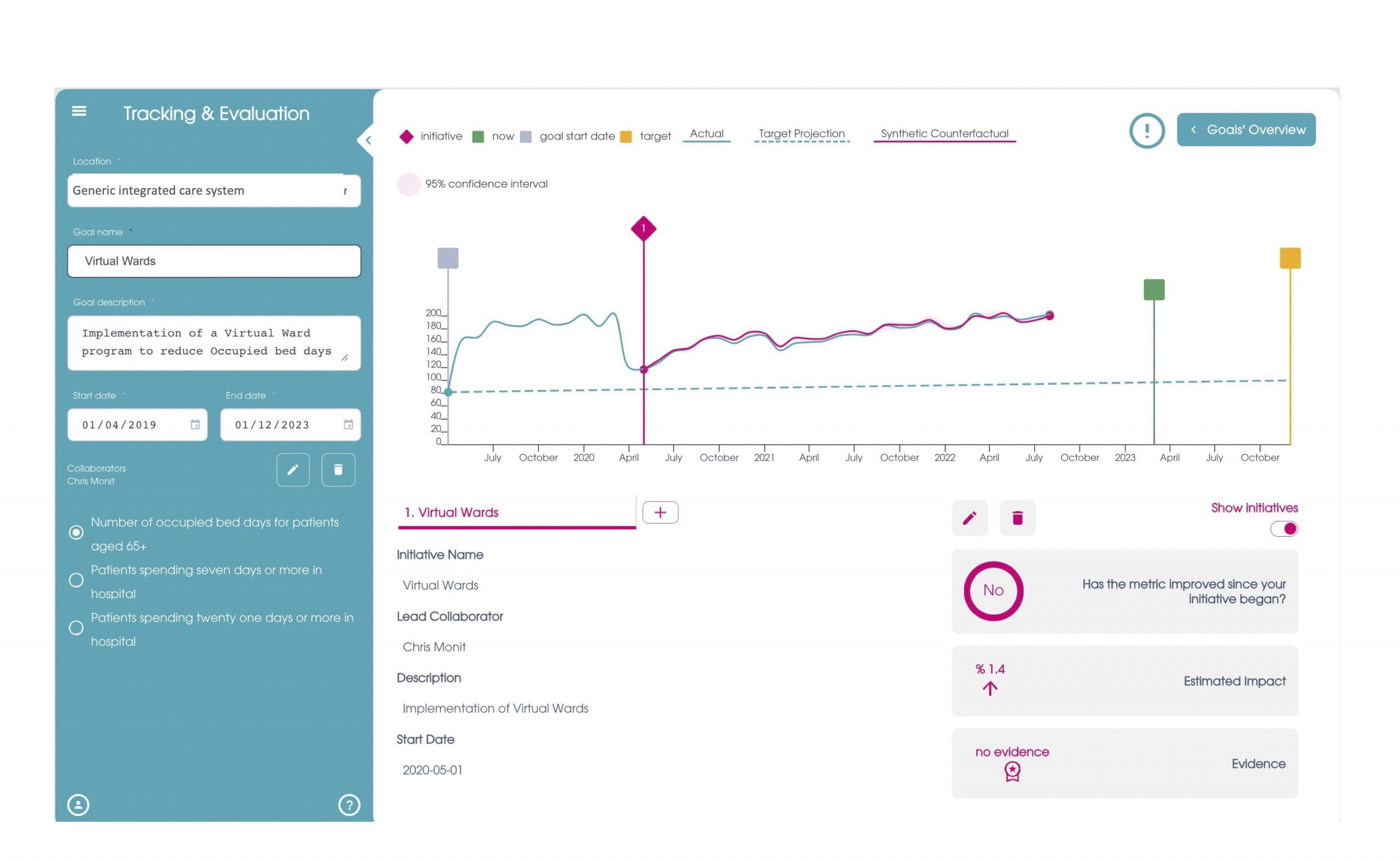
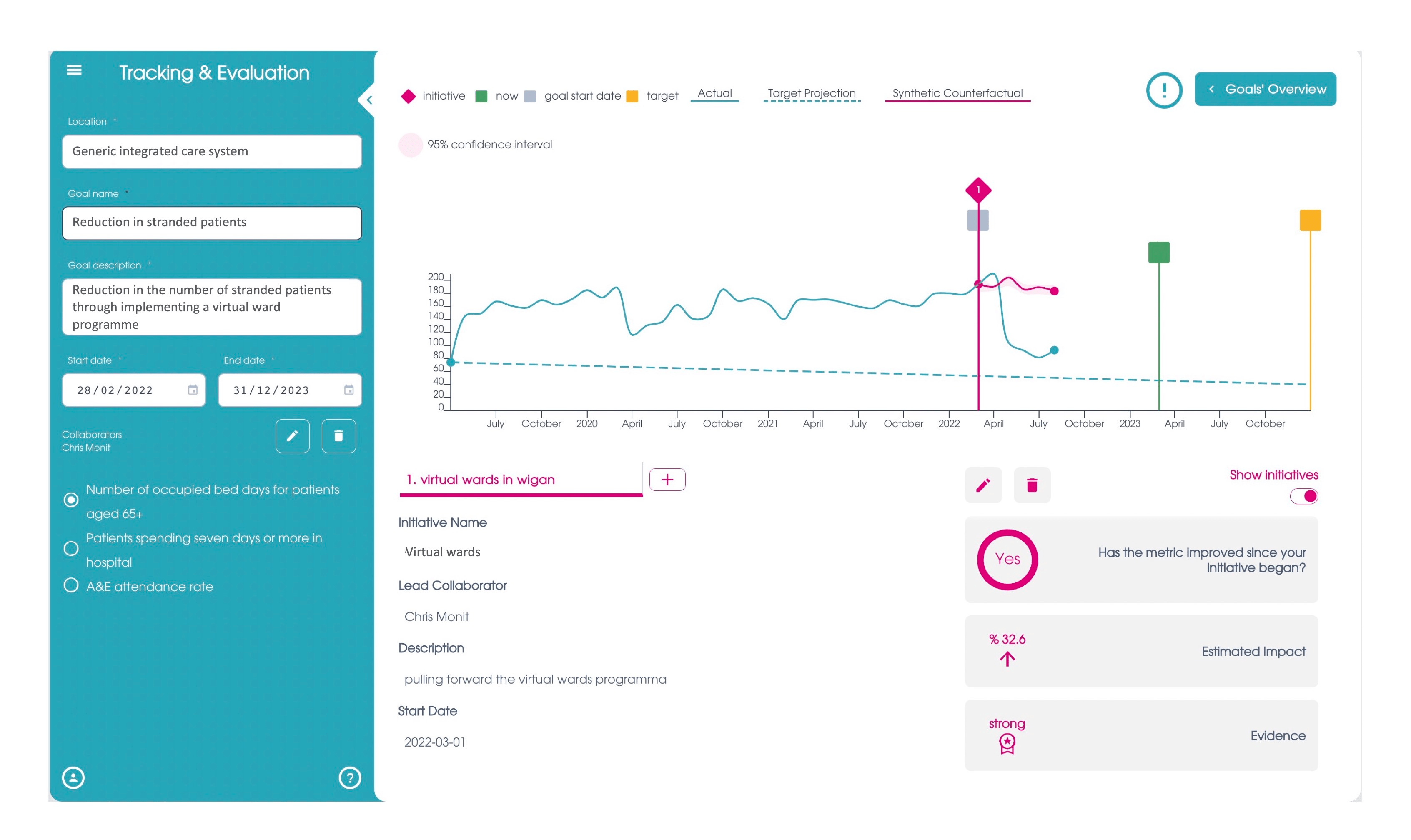
Our insight engine can be used to review the data available for metrics around virtual wards to assess their impact on a system, as set out in the examples above. There is a wide variation on the level of impact of virtual wards and it is important to monitor their effectiveness. If you would like to learn more, click here.
[1] NHSE. 2022/23 priorities and operational planning guidance. 2022. https://www.england.nhs.uk/wp-content/uploads/2022/02/20211223-B1160-2022-23-priorities-and-operational-planning-guidance-v3.2.pdf
[2] Lewis C, Moore Z, Doyle F, Martin A, Patton D, Nugent L (2017). A community virtual ward model to support older persons with complex health care and social care needs. Clin Interv Aging 12: 985–993;
[3] NHSX. 2022. Remote monitoring for patients with chronic conditions in the Midlands. [online] Available at: <https://www.nhsx.nhs.uk/covid-19-response/technology-nhs/remote-monitoring-for-patients-with-chronic-conditions-in-the-midlands/
[4] Swift, J. et al, 2022. An evaluation of a virtual COVID-19 ward to accelerate the supported discharge of patients from an acute hospital setting. British Journal of Healthcare Management, 28(1), pp.7-15.
[5] Schultz K, Vickery H, Campbell K, Wheeldon M, Barrett-Beck L, Rushbrook E (2021). Implementation of a virtual ward as a response to the COVID-19 pandemic. Aust Health Rev 45(4): 433–441. doi:10.1071/AH20240. PMID: 33840420.
[6] NHSE. Enablers for success: virtual wards including hospital at home. 2022. https://www.england.nhs.uk/wp-content/uploads/2022/04/B1382_supporting-information-for-integrated-care-system-leads_enablers-for-success_virtual-wards-including-hos.pdf
[7] Swift, J. et al, 2022. An evaluation of a virtual COVID-19 ward to accelerate the supported discharge of patients from an acute hospital setting. British Journal of Healthcare Management, 28(1), pp.7-15.
FULL CREDIT: Rhys Thomson, Will Fryer & Tom Brogden, carnallfarrar.com
YOU CAN GO TO THE FULL ARTICLE HERE: https://www.carnallfarrar.com/virtual-wards-why-and-how-to-make-them-a-success/